Energy fields sound “woo-woo.” Yet since ancient times, the stimulation of tissues—by massage, by needles with acupuncture, by heat and cold, and exercise—has been known to resolve tissue damage. The common pathway seems to be that all tissues are dynamic, constantly undergoing growth and resorption, their remodeling aided by the influx of cells, blood vessels, chemical stimulants, hormones, and small peptides.
The microenvironment of tissues—the cells and their biomacromolecules— all exhibit some level of sensitivity to sensory input. When physically “tickled,” they respond.
Certain musculoskeletal cells within injured tissues have been shown to have small filaments on their surfaces called mechanoreceptors. These cells respond to the stimulation of massage and other energy forms by increasing their metabolism, their collagen production, and their effectiveness at directing the healing response.
When a tissue (such as a muscle) is injured from a tear or a bruise, the immediate swelling we see is from the broken blood vessels bleeding into the area, and a release of fluid from the “extracellular space:” the area outside of the cells themselves. An alert, signaled by chemokines or small proteins, goes out to the body’s own stem cells, recruiting them to the site of injury to direct the healing response.
Specific cells, called monocytes, differentiate into several types of macrophages: those that break down the damaged tissues and others that release and organize new collagen fibers to rebuild the damaged structures. The swelling initially seen is the body’s immediate response. The longer the swelling persists, however, the slower the resolution of the healing. This is where the opportunity lies for external stimulation to be applied.
Shock waves, ultrasound, magnetic fields, red and laser lights, hot and cold energy from compression devices, and simple tissue massage all stimulate the mechanoreceptors, accelerating their activity. Some may directly affect the expression of local cell DNA. Even underlying bone cells, whether injured or arthritic, can respond to these energy applications. While initially thought to be useful only in acute injuries or non-healing bone lesions, newer data demonstrate that shock wave therapy slows the degradation in arthritic joints by stalling the cell cycle of the osteoblast and diminishing their trajectory to cell death1.
Cells that are senescent (dead) from injury or chronic arthritis secrete inflammatory proteins, accelerating the osteoarthritis disease. Removing them—or diminishing their progress by shock wave therapy—has been shown to be of benefit in cartilage, rotator cuff, and meniscus repair2.
The use of heat and cold, red lights and lasers, ultrasound, and magnetic fields all function by the same basic mechanism: stimulation of tissues. Shock wave therapy appears to be the most energetic of the applications and may work by actually creating a new injury, a shearing injury of the tissues with the acoustic waves, thereby sending new chemotactic signals to recruit stem cells. Though the scientific data on each modality is all over the place, and the frequencies, dosages, and intervals are completely uncontrolled in studies, the principle of safe tissue stimulation remains both viable and exciting.
Massage of tissues with hands or devices, ice and heat, and exercise, all have positive effects on the healing cycle and are the least expensive of the interventions. The challenge is to provide just the right amount of stimulation at the right moment in a cost-effective and time-efficient manner.
Similar to the best energy policy at the government level, an all-of-the-above approach seems the best strategy for healing injuries this time.
References
- Chen L, Zhang Z, Ma X, Zhang D, Xu Q, Wang Q, Pan S, He Y & Liu X. Radial Extracorporeal Shockwave Therapy Reduces Subchondral Osteoblast Senescence in Knee Osteoarthritis. The American Journal of Sports Medicine. 2025;53(10):2352–2362. doi:10.1177/03635465251355245
- Jhan SW, Wang CJ, Wu KT, Siu KK, Ko JY, Huang WC, Chou WY & Cheng JH. Comparison of Extracorporeal Shockwave Therapy with Non-Steroid Anti-Inflammatory Drugs and Intra-articular Hyaluronic Acid Injection for Early Osteoarthritis of the Knees. Biomedicines. 2022;10(2):202. doi:10.3390/biomedicines10020202
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.
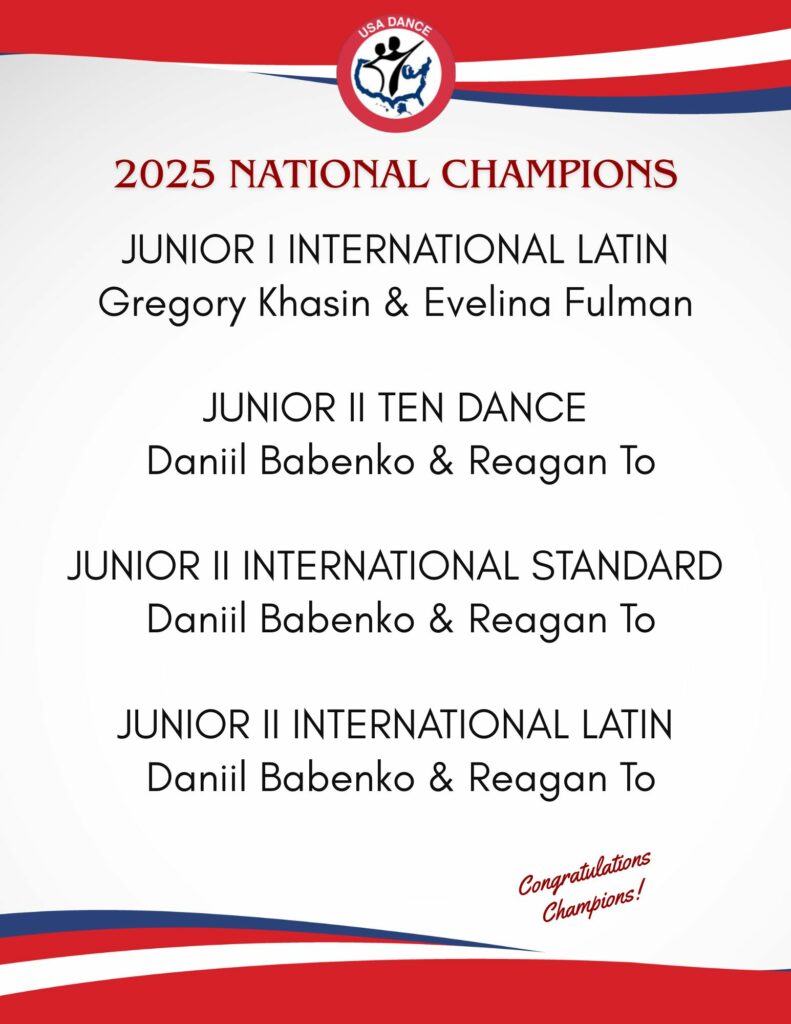
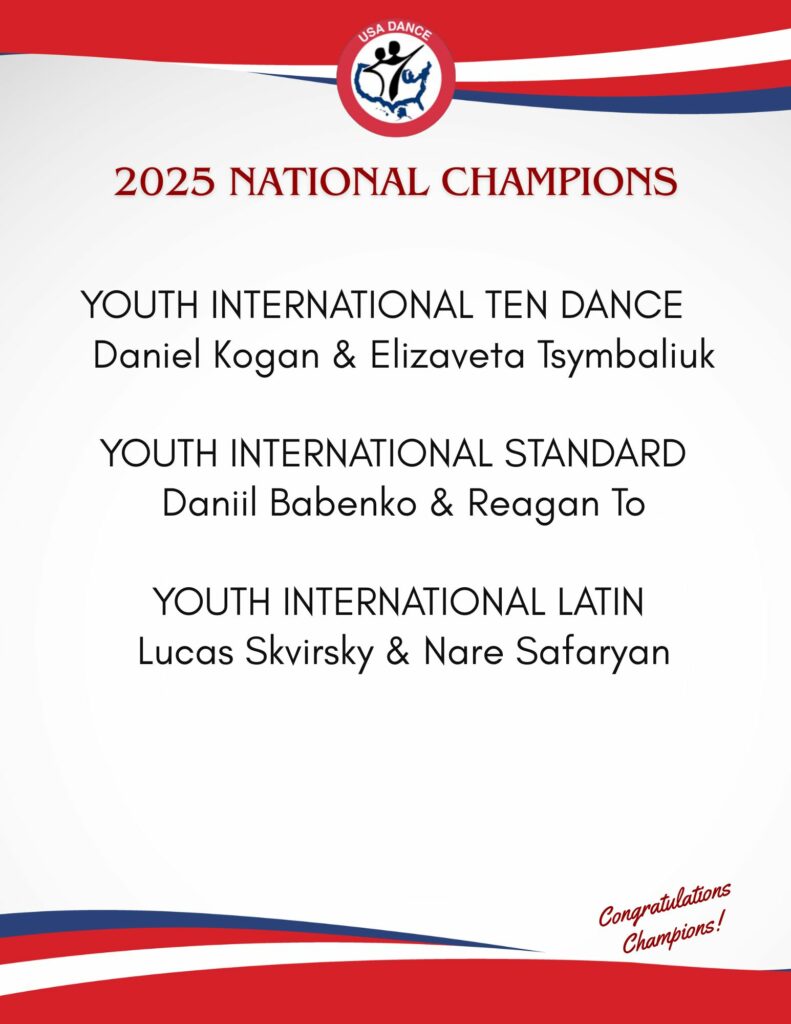
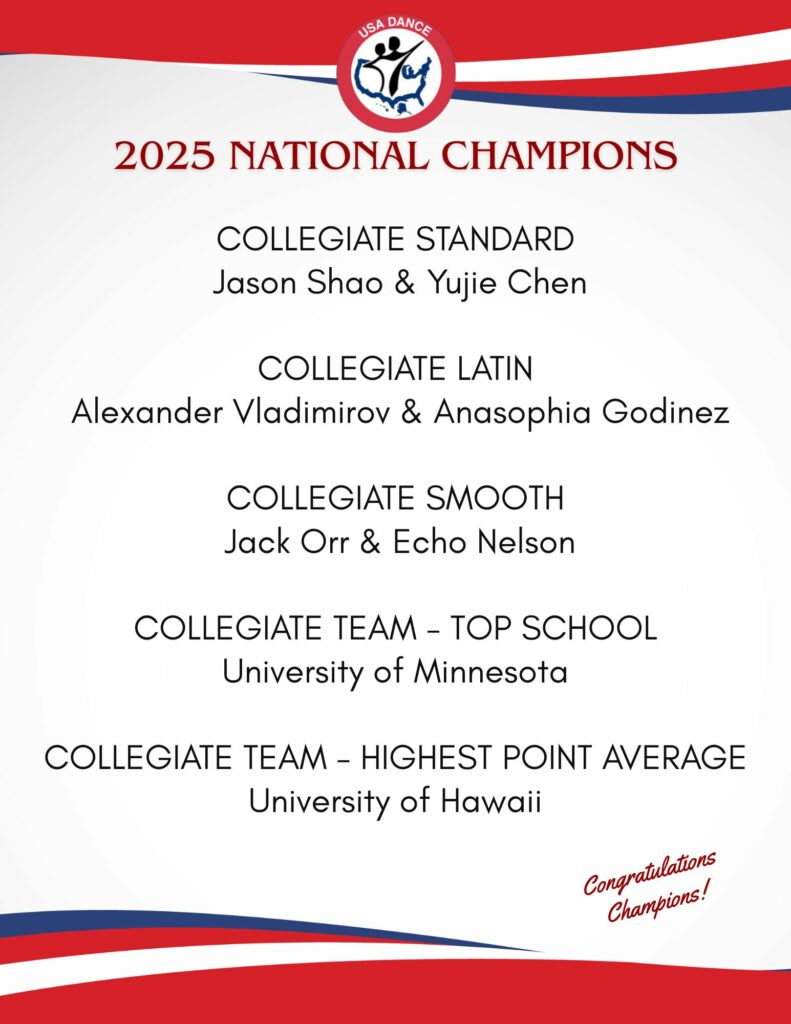
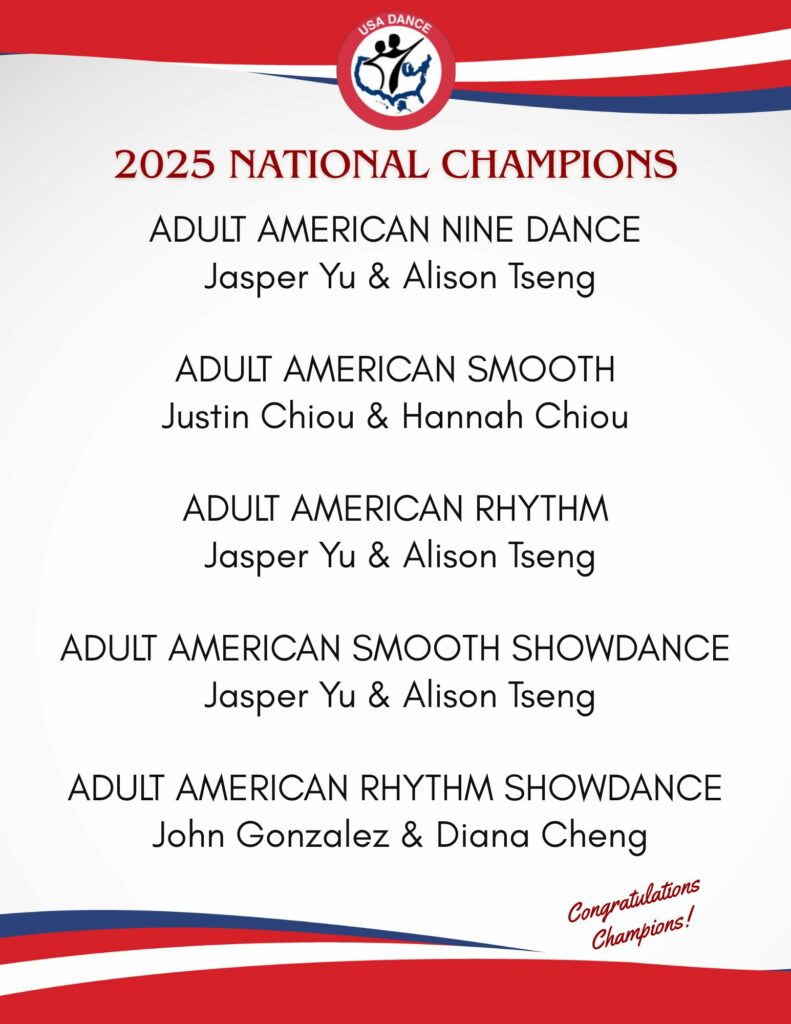
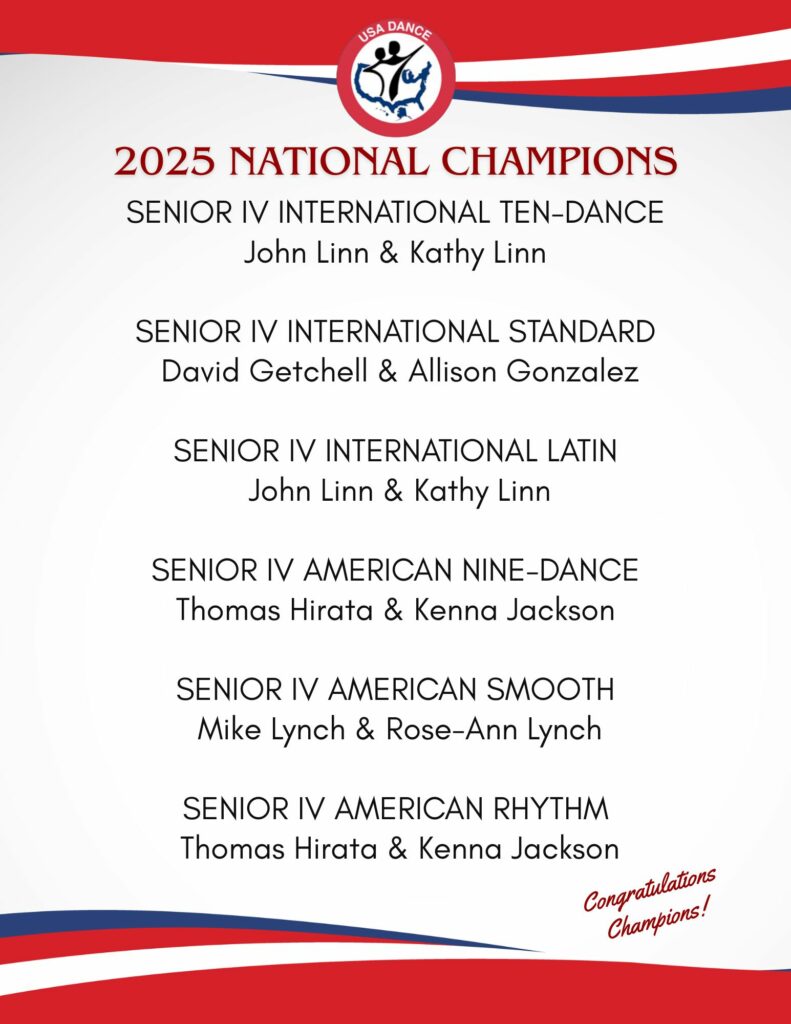
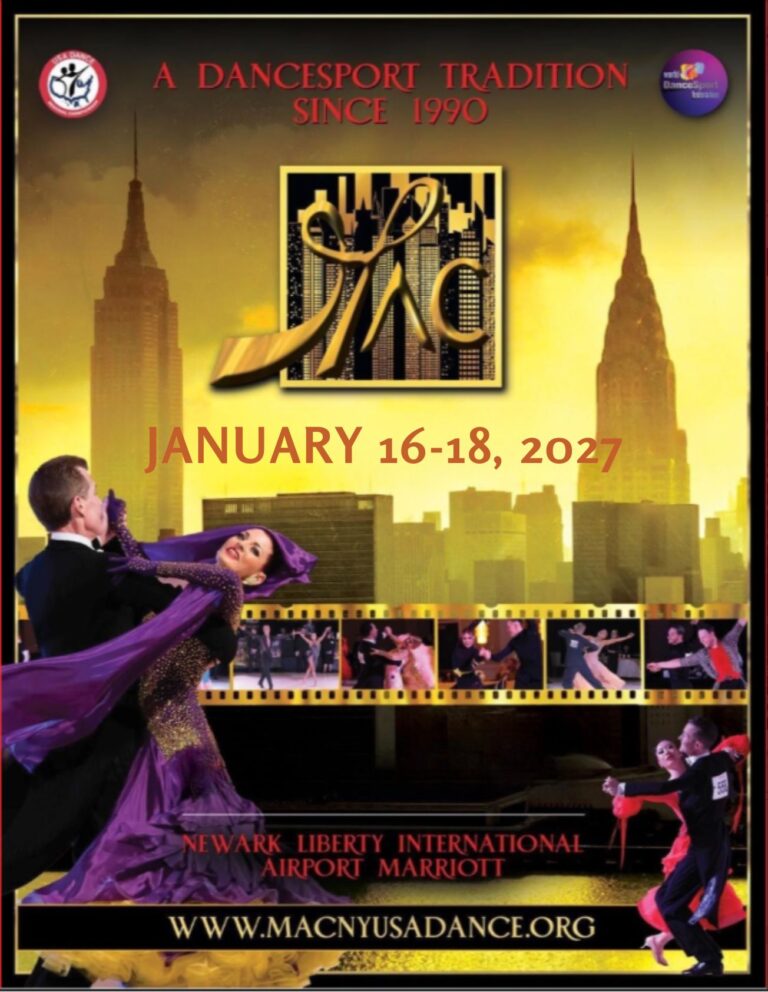
Editor’s Note: Thank you to Dr. Kevin Stone and the Stone Clinic for allowing American Dancer to republish his articles. Read about one of our National Champions’ experiences with a knee replacement by Dr. Stone at the Stone Clinic. Link: Senior III and IV Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. Mike also provides a checklist to help you if you travel for surgery. Since his partial knee replacement, Mike has won three USA Dance National Championship titles.
Dr. Stone is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!