“Overuse injury” is the throw-away term given to a wide range of injuries that athletes—especially young athletes—suffer. Symptoms of overuse injury include: Pain, swelling, and decreased athletic performance. The medical literature lists huge numbers of cases. Here is the typical information people are given about overuse injuries:
Overuse injuries represent 30-50% of all sports-related injuries in young athletes, with one in three requiring medical attention. The ankle and knee are the most commonly injured, followed by the elbow, depending on the sport the athlete is playing.
The most common diagnoses are:
- Osgood-Schlatter disease: Pain at the growth plate on the front of the tibia.
- Jumper’s Knee: Patellar tendon pain.
- Medial epicondylitis: Pain at the bony bump on the inside of the elbow.
- Osteochondritis dissecans: Loosening of cartilage and bone, most commonly in the knee and ankle.
- Sever’s disease: growth plate pain at the calcaneus (heel bone).
- For adolescent baseball players: elbow and shoulder pain, commonly thought to be variously related to age, height, number of teams played for, pitch velocity, and arm fatigue. Often, these young players are found to have external and internal rotation muscle weakness and lost range of motion.
Unfortunately, the most frequently recommended treatment is rest.
It is our belief that the single common denominator in all of these diagnoses is an initial tissue injury. At the time of the injury, the collagen fibers of the tendon, or of the articular cartilage of the joint, suffer a tearing, or the bone underlying these areas is fractured. Instead of healing promptly, the site of injury follows a pathway of chronic inflammation, degeneration of the now-abnormal tissue, and formation of a painful site. In our view, it is the injury that is the primary problem in most cases, not the volume of pivots, the repetition of pitches, or the rapid pace of the athlete’s growth.
Once this philosophy is accepted, the solutions can follow a more normal course of diagnosis, treatment, and recovery. For instance, a painful patellar tendon in an adolescent basketball player or a sore elbow in a young pitcher most likely resulted from a tear in the critical collagen fibers, which make up the core of the tendon itself. An immediate MRI would reveal the torn fibers. All professional athletes would get one. Treatment would include some combination of stimulation of the collagen to heal—possibly with massage, energy (e.g. ultrasound, magnetic fields), heat, cold, and others.
Other treatment options might include injection therapies, including PRP (currently) and, in the near future, specialized packets of growth factors (exosomes), peptides, or birth tissues (Wharton’s Jelly), which have sixty times the growth factor concentrations of PRP alone. The data for these anabolic injections is not yet definitive, and not yet widely applied to children, and the costs are considerable. However, the cost of losing one or more seasons due to an “overuse” injury, or even surgery for “overused” tendons, is not trivial.
A pro athlete has their career and economic viability on the line with each injury. They bring everything to the table to treat injuries, followed by optimal nutrition, massage therapy, physical therapy, and application of all available tissue stimulation devices in order to speed recovery as rapidly as possible.
If we applied even some of this approach (within economic reason) to children, their lives and the lives of their parents and coaches would be freed from months or years of just “resting the injury” and hoping for the best.
References
- Gibson ES, Cairo A, Räisänen AM, Kuntze C, Emery CA, Pasanen K. The Epidemiology of Youth Sport-Related Shoulder Injuries: A Systematic Review. Trans Sports Med. 2022 Aug 23;2022:8791398. PMID: 38655170; PMCID: PMC11022765. doi:10.1155/2022/8791398
- Mohr B, Mabrouk A, Blade JD. Osteochondritis Dissecans of the Knee. [Updated 2024 Jan 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538194/
- Norton R, Honstad C, Joshi R, Silvis M, Chinchilli V, Dhawan A. Risk Factors for Elbow and Shoulder Injuries in Adolescent Baseball Players: A Systematic Review. The American Journal of Sports Medicine. 2018;47(4):982–990. doi:10.1177/0363546518760573
- Trofa DP, Obana KK, Swindell HW, Shiu B, Noticewala MS, Popkin CA, Ahmad CS. Increasing Burden of Youth Baseball Elbow Injuries in US Emergency Departments. Orthop J Sports Med. 2019 May 14;7(5):2325967119845636. PMID: 31205966; PMCID: PMC6537065. doi:10.1177/2325967119845636
- Leppänen M, Pasanen K, Kujala UM, Parkkari J. Overuse injuries in youth basketball and floorball. Open Access J Sports Med. 2015 May 22;6:173–179. PMID: 26045679; PMCID: PMC4447174. doi:10.2147/OAJSM.S82305
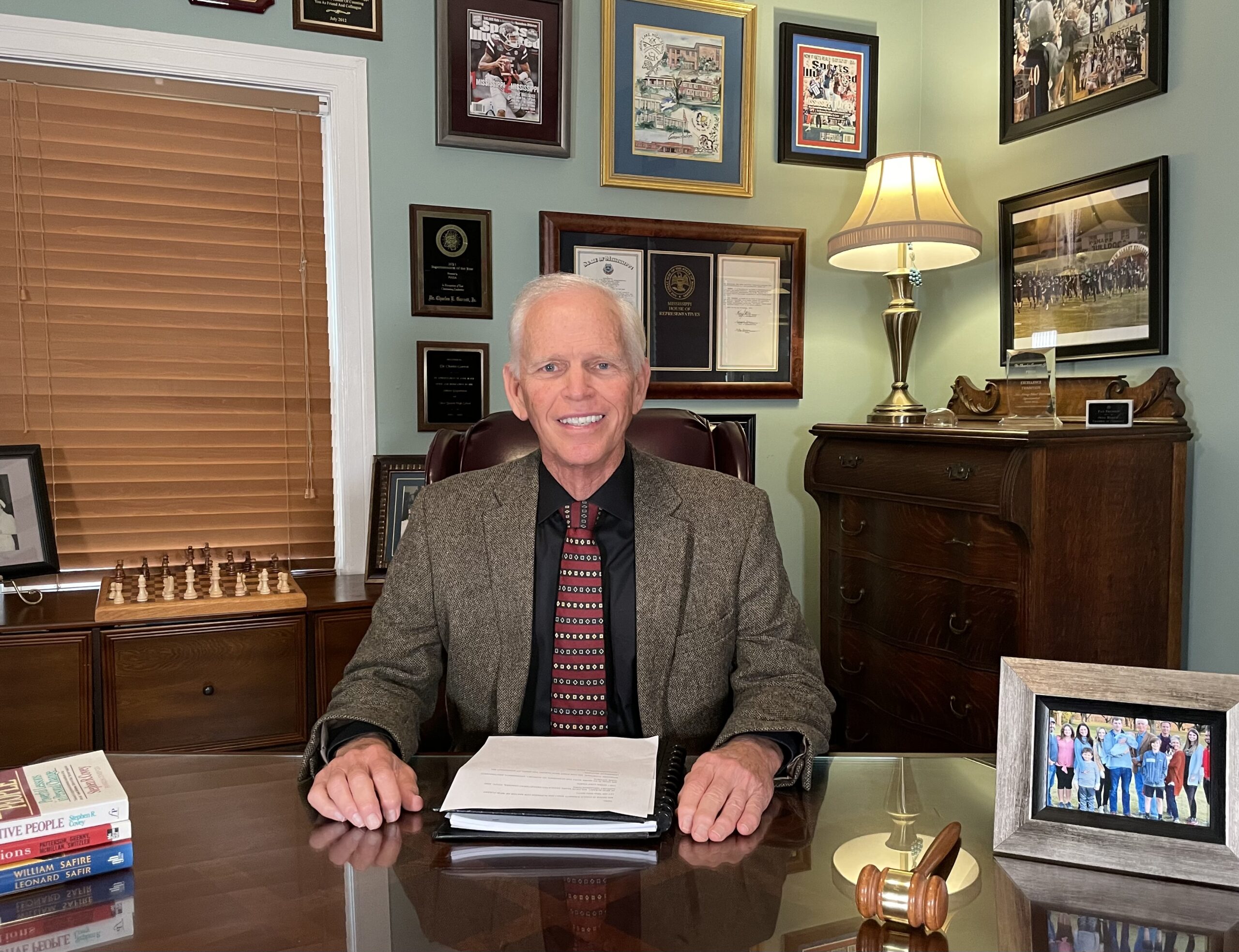
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.
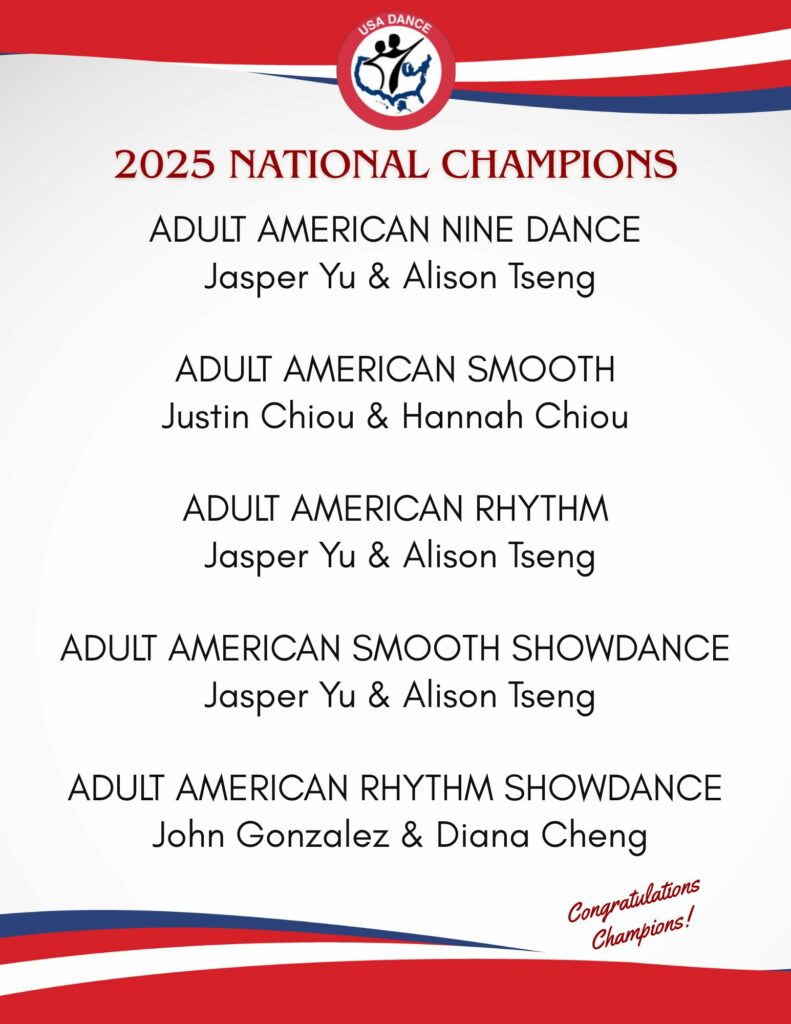
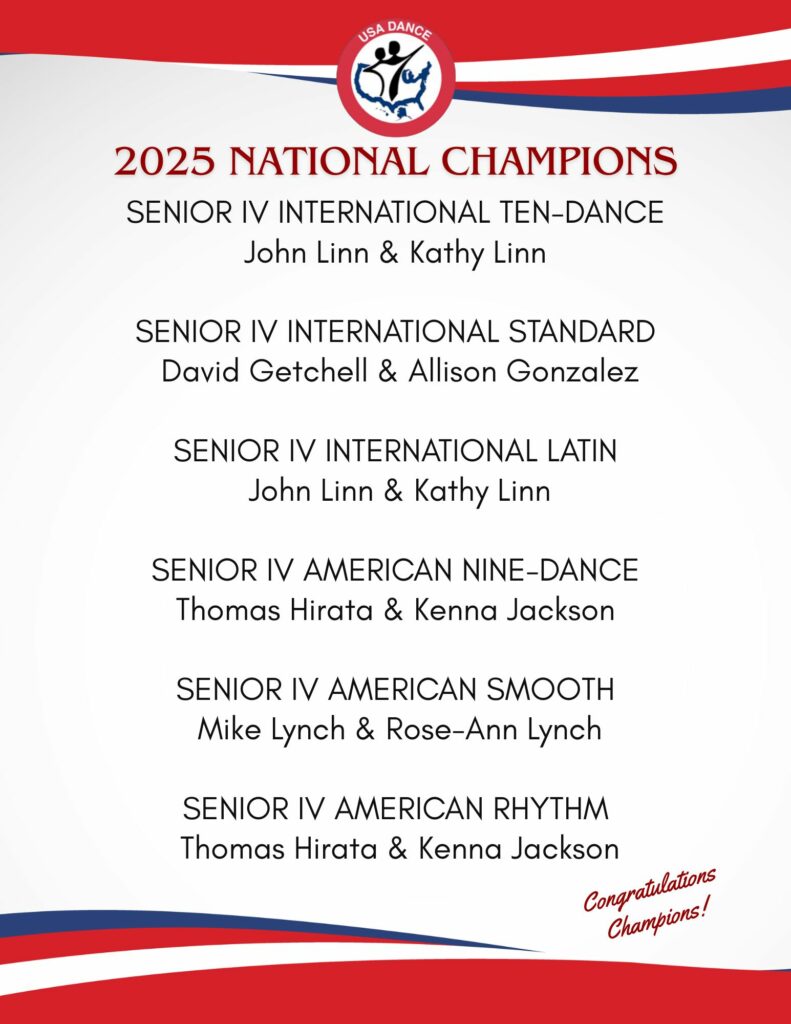
Editor’s Note: Thank you to Dr. Kevin Stone and the Stone Clinic for allowing American Dancer to republish his articles. Read about one of our National Champions’ experiences with a knee replacement by Dr. Stone at the Stone Clinic. Link: Senior III and IV Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. Mike also provides a checklist to help you if you travel for surgery. Since his partial knee replacement, Mike has won three USA Dance National Championship titles.
Dr. Stone is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!