1. NPO (i.e., eating or drinking) after midnight
This long-held philosophy, unfortunately, leaves you going into surgery dehydrated and feeling dried out. While in surgery, the amount of fluid you are given through your IV varies widely. Hydrating well the day before surgery and using electrolyte-rich fluids like Gatorade post-surgery will help you regain your normal fluid status and speed your recovery. Expect to get up at night to pee more often than normal, even though you are dry. Sleep near a bathroom.
2. Pain
Pain is not your friend and is not beneficial after surgery. Preemptive anesthesia means loading your tissues and your body with drugs that prevent your brain from getting the pain signals in the first place. Many strategies exist, but the most popular are a combination of non-steroidal anti-inflammatory drugs (NSAIDs) the night before, regional nerve blocks placed in the pre-op area, IV Tylenol and Ketorolac (Toradol), which block various pain receptors, and local injection into the tissues with long-acting Novocain-like drugs before any incision is made. Re-injection of novel compounds made of these long-acting drugs, combined into slowly absorbing gels with additional anti-inflammatories, can be placed deep into the tissues before the wounds are closed. The use of tranexamic acid (TXA) before surgery has been shown to reduce bleeding, swelling, and pain both during surgery and in the recovery period. This drug has eliminated the use of tourniquets in our practice. Tourniquets were a major source of post-op pain and muscle inhibition. Additionally, almost everyone should use a stool softener or a GI bomb (a combination of olive oil plus prunes, plus caffeine) since post-op constipation can produce significant abdominal discomfort.
3. Physical therapy
Many doctors and insurance companies discourage immediate physical therapy, yet we have found it to be critical to a rapid and comfortable recovery. Soft tissue massage on the affected extremity diminishes swelling (swelling equals more pain and slower healing). Immediate, day-one post-op PT also permits the patient to start a supervised exercise program. The operated leg can be stabilized on a chair while a stationary bike is ridden or a rowing machine is used with a slider on the floor. Raising the heart rate early helps flush the anesthesia drugs from the body and increases testosterone, pheromones, adrenaline, and endorphins — all improving patient outlook and diminishing operative site pain. We want you to see yourself as an athlete in training, not as a patient in rehab. Athletes do better with coaches. The rehab team therapists are pros at coaching the recovery process.
4. Mind preparation
The Buddhist philosophy that “Pain may be inevitable. Suffering is optional” can inspire you to think about the upcoming surgery with acceptance and determination. Recognize the discomfort, the intrusion in your life, the loss of time with friends and family, and compel yourself to adopt an athlete’s mindset: that the challenge ahead is doable and tolerable.
5. Support team
Lining up a great support team for your procedure makes an enormous difference. Support from family and friends, trainers and physical therapists, and even colleagues at work sets the stage for a team effort and successful outcome.
6. Novel drugs
Even our 80-year-old patients are using nighttime THC/CBD gummies or equivalents for sleep and to reduce the post-op use of narcotics. Though we cannot yet prescribe them, they appear to be quite effective. JournaVax is a new peripheral pain reliever that doesn’t make you sleepy and may become widespread if the costs come down. Toradol (Ketorolac) plus Tylenol post-op is our preferred combination before a patient tries any narcotic.
7. Ice compression machines
These tools work to sequentially compress, chill, and release the tissues. Used 20 minutes per hour, they reduce swelling and pain.
8. Motion
Motion is almost always your friend. Check with your doctor on how much you can move your operated area. In general, early motion is preferred to reduce stiffness and scarring. Casts and braces are used rarely now as they clearly produce what we call “brace disease,” the loss of motion after surgery.
9. Avoid infection
Infections are relatively rare in high-quality surgical environments, but they can happen to anyone. The biology of the patient probably matters the most. We could literally spit in one patient’s knee and they would never get an infection, while another patient would be infected by a single microbe landing from the air. Coming to surgery well nourished (low albumin leads to high infection rates), well hydrated, off any corticosteroids (a single shot of cortisone within three months of surgery has been shown to raise infection rates), with a well cleaned body (chlorhexidine soap the night before and the morning of surgery works), and never touching the post-op wound are good ways to reduce infections. Everyone has E.coli bacteria on their thighs after they use the toilet to pass stool. Touching your thigh and then touching your wound is a common source of infection. We use tight suture closures, skin glue, adhesive wound dressings, and waterproof clear dressings like Tegaderm or Opsite to prevent the patient from getting to the incisions. This defense needs to be kept up, if possible, for two to three weeks after surgery. If an infection does occur, rapid and accurate diagnosis is essential prior to any antibiotic use. If antibiotics are taken before a culture is taken, it is very difficult to determine which antibiotic to use and for how long. Immediate aspirations or wound cultures, with prompt surgical irrigation followed by antibiotics, can cure most infections. Keeping a positive outlook and working closely with your surgical and infectious disease team are core principles to reaching a healthy state again.
10. Injury and surgery are opportunities
If you line up your best recovery team, optimize your nutrition, hire a trainer and a physical therapist, and set your goal at getting back better than you were before you were injured, you can achieve your dreams — and ours.
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.
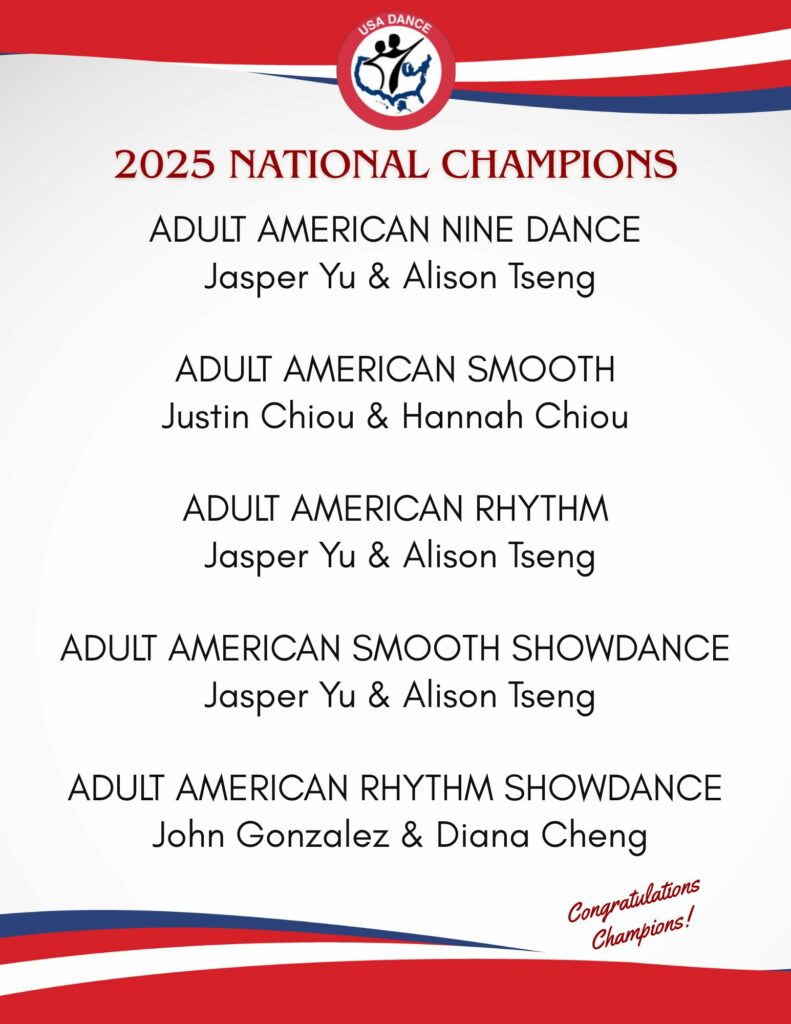
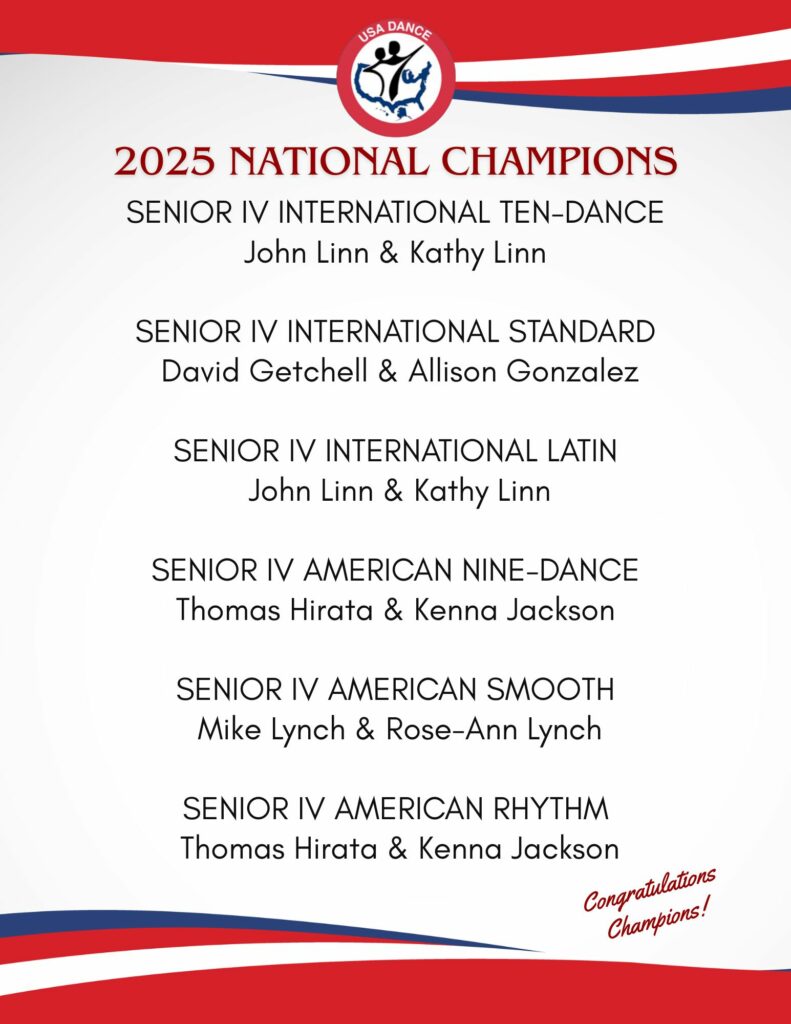
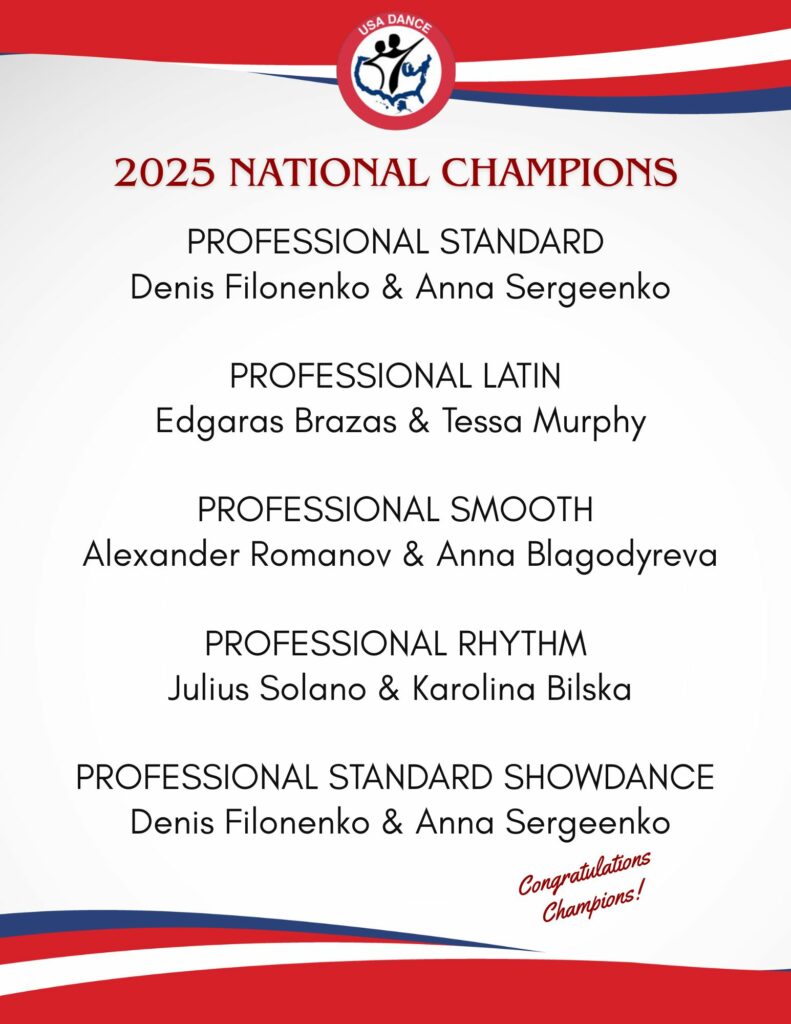
Editor’s Note: Thank you to Dr. Kevin Stone and the Stone Clinic for allowing American Dancer to republish his articles. Read about one of our National Champions’ experiences with a knee replacement by Dr. Stone at the Stone Clinic. Link: Senior III Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. Mike also provides a checklist to help you if you travel for surgery.
Dr. Stone is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!