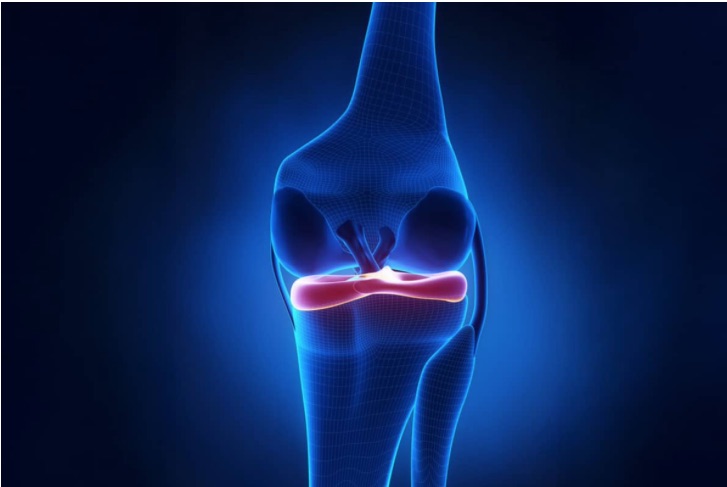
Everyone now recognizes that the meniscus is important to save. Yet few save it fully, and even fewer replace it. Here are a few of the most recent debates, highlights, and lowlights from the recent international meeting, ISAKOS (International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine) in Munich in June 2025:
Meniscus repair is easier than ever. Devices have now been made that permit many of the most difficult-to-reach tears to be sewn together with “all inside” devices, eliminating the need for an assistant or a separate incision. All the companies sell variations of these devices.
The problem is that the devices are expensive when compared to suture and fail up to 30% of the time. They use a relatively large insertion needle that can damage the healthy meniscus and incorporate an artificial implant to hold the torn edges in place. Some use a folding knot at the back of the knee. Any of these can come loose and damage the knee. The older technique of direct suture repair is taught less, since the implant companies don’t profit from it—and the teaching sessions at the meetings are all sponsored by the implant companies.
Meniscus tears at the root of the meniscus are now recognized as fatal to the overall meniscus function. Root repair techniques have improved.
Techniques to reduce the torn meniscus back to the bone where it inserts have evolved. There are now instruments and implants for the surgeon to use. Unfortunately, they are also expensive—and because the meniscus ruptured in the first place, the quality of the tissue is suspect and most likely degenerative. Sewing damaged tissues back to bone has a high failure rate. There remains an open opportunity for innovation.
Meniscus tears at the ramp of the meniscus within the meniscal tibial ligaments are now known to lead to ACL reconstruction failure due to residual laxity of the knee.
Beautifully shown by Smigelski in anatomic studies and by Sonnery-Cottet in clinical outcome studies, the meniscus is attached to the tibia by strong meniscus tibial ligaments. When an ACL tears, the forces that drive the tibia away from the femur tear not just the ACL fibers but the meniscus ligament fibers as well. Failure to recognize and repair these leads to ongoing problems for patients. These repairs, however, take time, and a surprising number of surgeons are not comfortable operating in the back of the knee during arthroscopic procedures.
Loss of the lateral meniscus from tears and surgery is recognized to be fatal to the knee joint, especially in young people. Many surgeons confront torn lateral meniscus tissue when they find a discoid or dish-shaped meniscus in young patients. But shaping these developmentally abnormal tissues often fails due to the abnormal organization of the collagen fibers in the discoid meniscus.
Loss of the lateral meniscus in a young person is an obvious, urgent call for a meniscus replacement. Loss of a significant amount of any meniscus tissue in people of all ages raises the question: Should a donor meniscus be put back in? And if so, when? Our biasis to replace the meniscus as soon as possible to save the knee. We have published our findings that meniscus replacement, even in patients over 50 years of age with arthritis, can delay or prevent an artificial joint replacement. However, it is far better to prevent degenerative arthritis in the first place. Yet while over 800,000 menisci are removed in the US each year, only 20% are repaired and less than 3,000 are replaced1,2. Cost, technical ability of the surgeon, tissue availability, and insurance reimbursement are most often cited for this disparity.
Partial meniscus replacement
Many recognize that small amounts of the meniscus, when resected in the posterior part of the medial meniscus, lead to failure of the entire meniscus to protect the joint. Rather than replace the entire structure, efforts have been made to restore part of it. Portions of tissues from allografts and sections of the patient’s own tendons were presented again (as they were in the 1980s) as possible solutions for segmental restoration of the resected meniscus, though without any significant follow-ups. The collagen meniscus implant scaffolds that I was fortunate enough to invent in 1986 for meniscus are now off the market—but will come back soon with new and improved constructions.
Injections of PRP, exosomes, and stem cells are growing in popularity.
Though no data has shown that any of these regrows tissues, all of the biologic injectionsappear to improve symptoms—probably by reducing inflammation, stimulating the lining cells of the joint to produce more natural lubricants, and recruiting the patients’ own stores of stem cells. This latter mechanism, including the shifting of specialized repair cells called macrophages, from one inflammatory state to another more constructive state, most likely explains the long-term effects on joint health of even a single injection. Injections of these combined growth factors, lubricants, anabolic, and chemotactic attractants are the fastest and most promising aspect of optimizing joint health, and possibly treating or preventing arthritis. We remain optimistic and are actively testing and using some of these therapies.
Nothing grows faster than the fetus. The reason the mother’s body does not reject the fetus, even though the fetus has only half the mother’s genes, has to do in part with the therapeutic factors in the amniotic fluid, Wharton’s Jelly, and related membranes. Surgeons, as far back as the 1910s, used birth tissues to reduce scarring. The anti-fibrotic and anabolic features of these tissues, as well as their ability to stimulate tissues while not causing scarring in abdominal surgery3,4,5 are unique to these components. Though birth tissues may be the most potent source of all of these factors, they currently remain restricted by the FDA. That is unfortunate—if there is a fountain of youth, we expect to find it there.
References
1. Kahan JB, Burroughs P, Petit L, et al. Rates of subsequent surgeries after meniscus repair with and without concurrent anterior cruciate ligament reconstruction. PLoS One. 2023;18(11):e0294964. Published 2023 Nov 28. doi:10.1371/journal.pone.0294964
2. De Bruycker M, Verdonk PCM, Verdonk RC. Meniscal allograft transplantation: a meta-analysis. SICOT J. 2017;3:33. doi:10.1051/sicotj/2017016
3. Davis JS. Skin grafting at the Johns Hopkins Hospital. Annals of Surgery. 1909;50(3):542-549. doi:10.1097/00000658-190909000-00002
4. Sabella, N. Use of fetal membranes in skin grafting. Medication Reconciliation in New York. 1913;83:478.
5. Parmar UP, Surico PL, Scarabosio A, et al. Amniotic membrane transplantation for wound healing, tissue regeneration and immune modulation. Stem Cell Reviews and Reports. 2025. doi:10.1007/s12015-025-10892-x
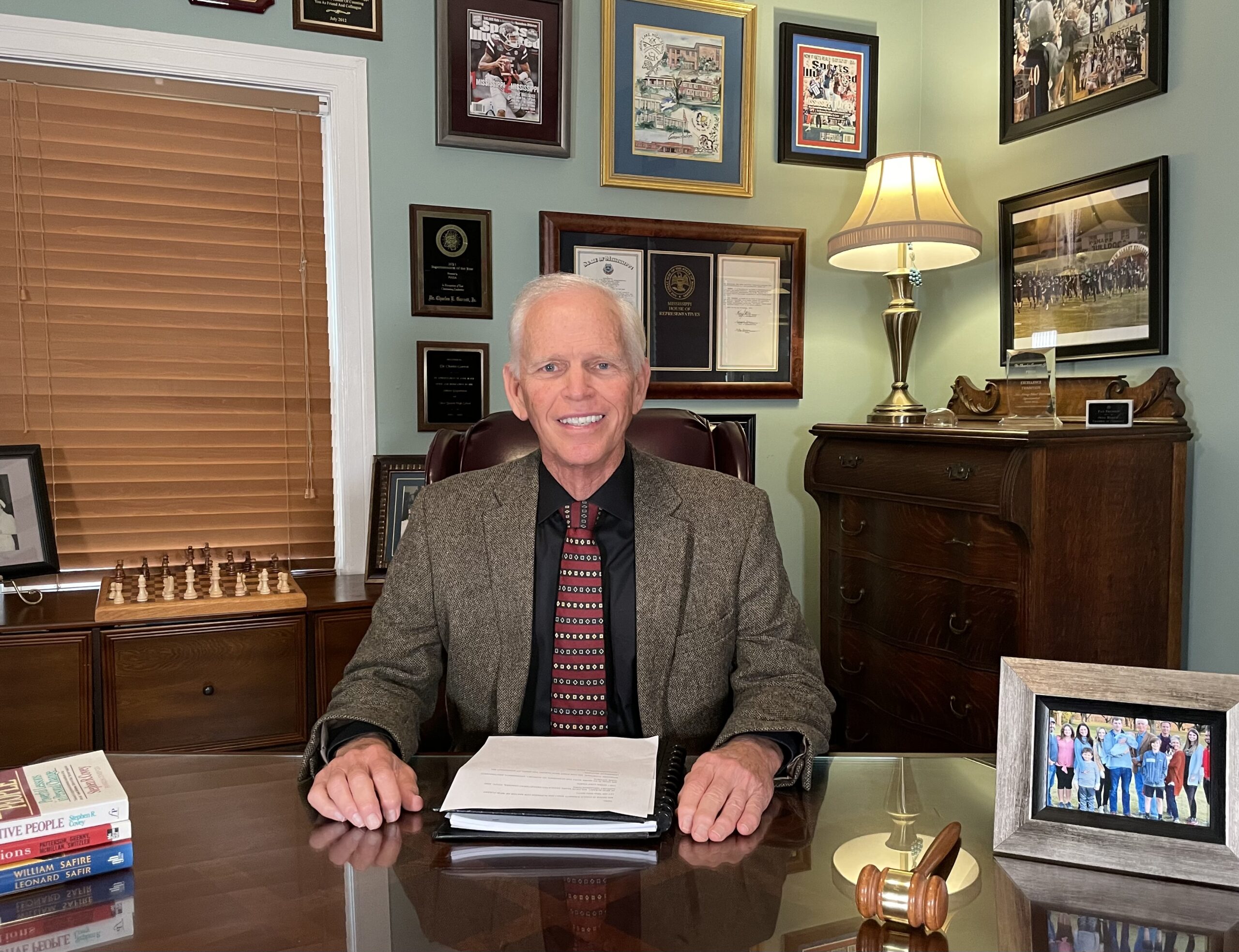
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.
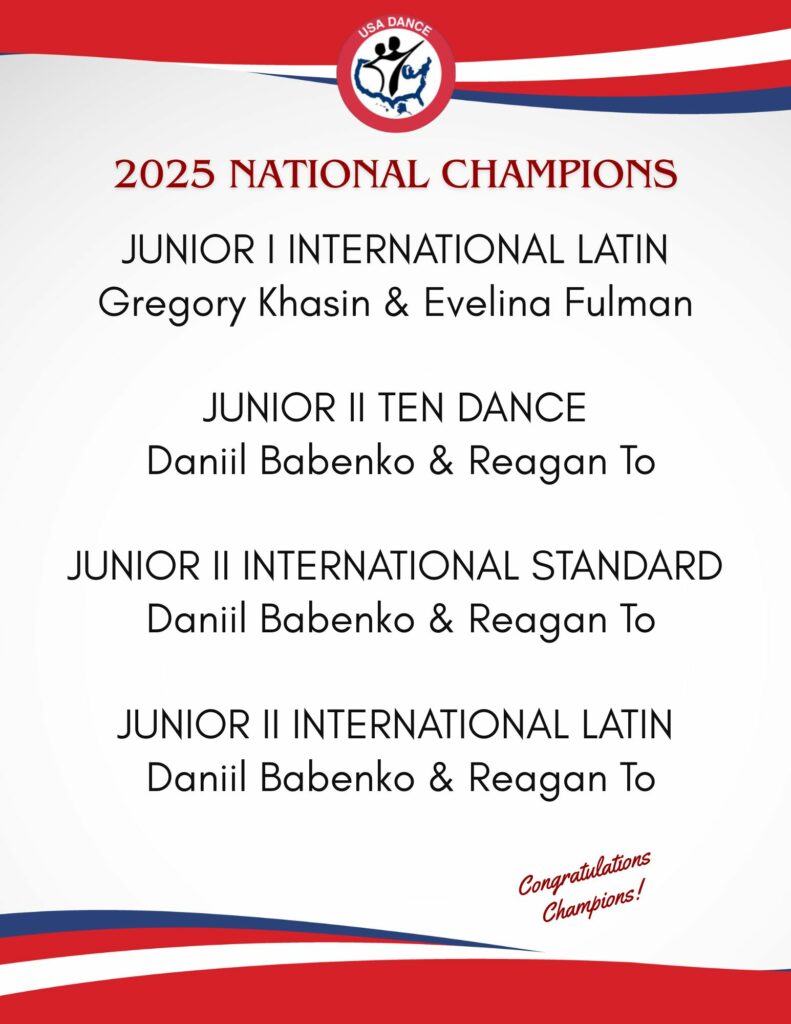
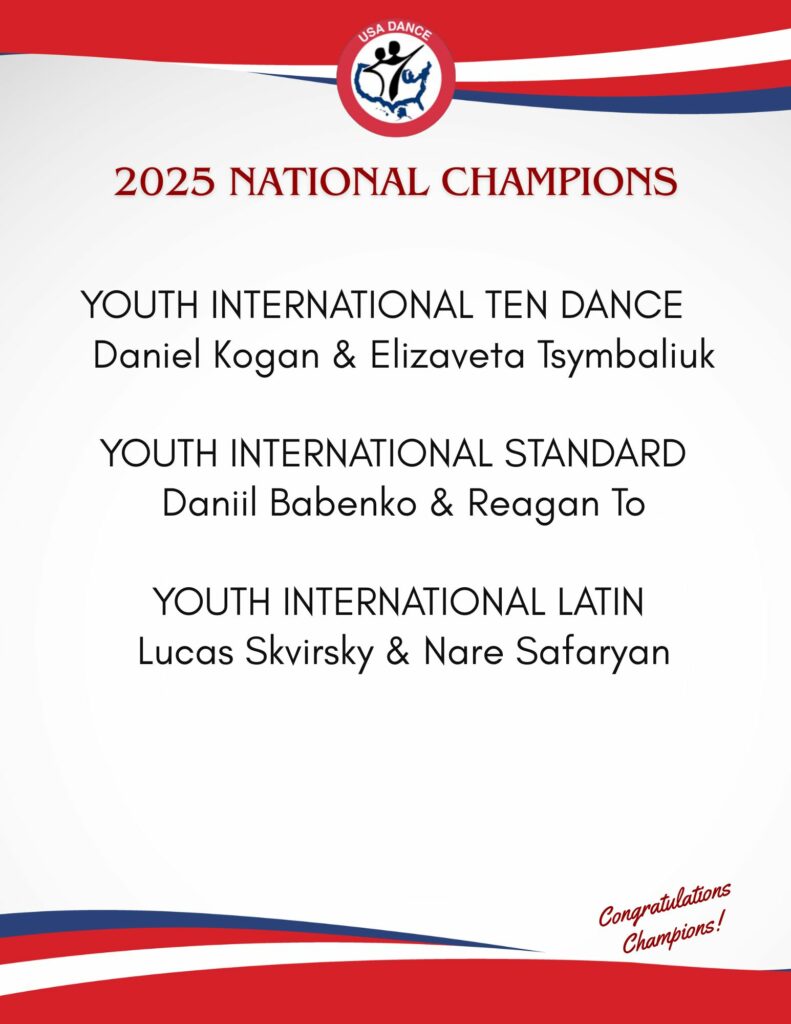
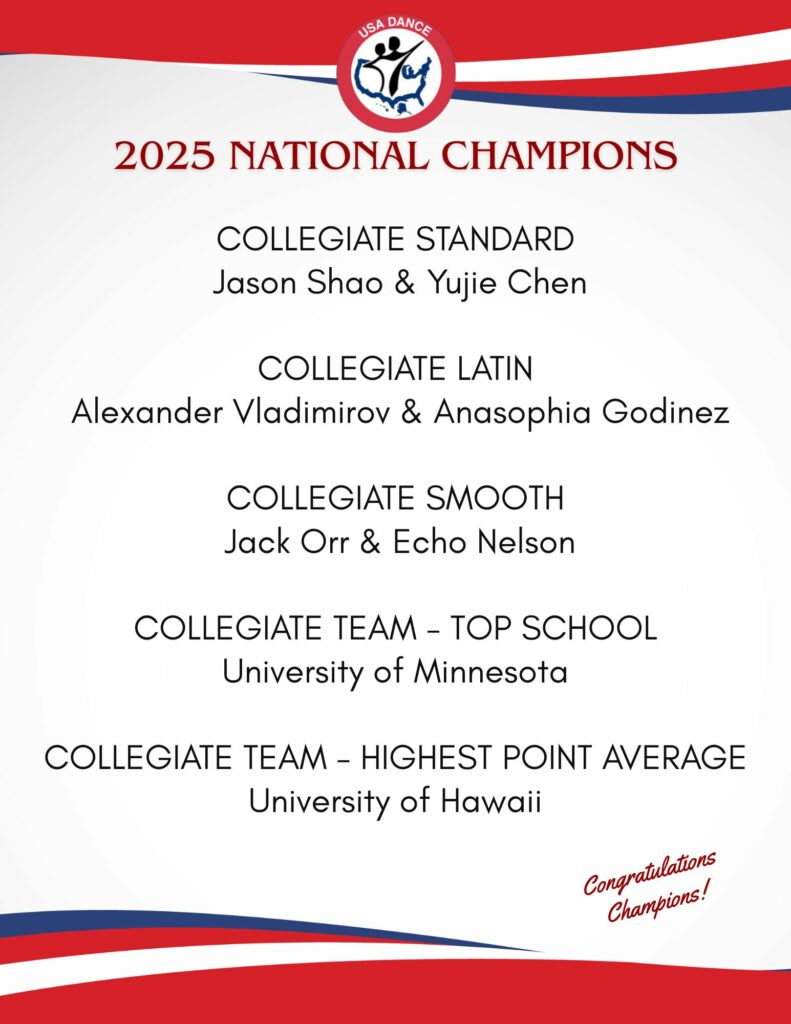
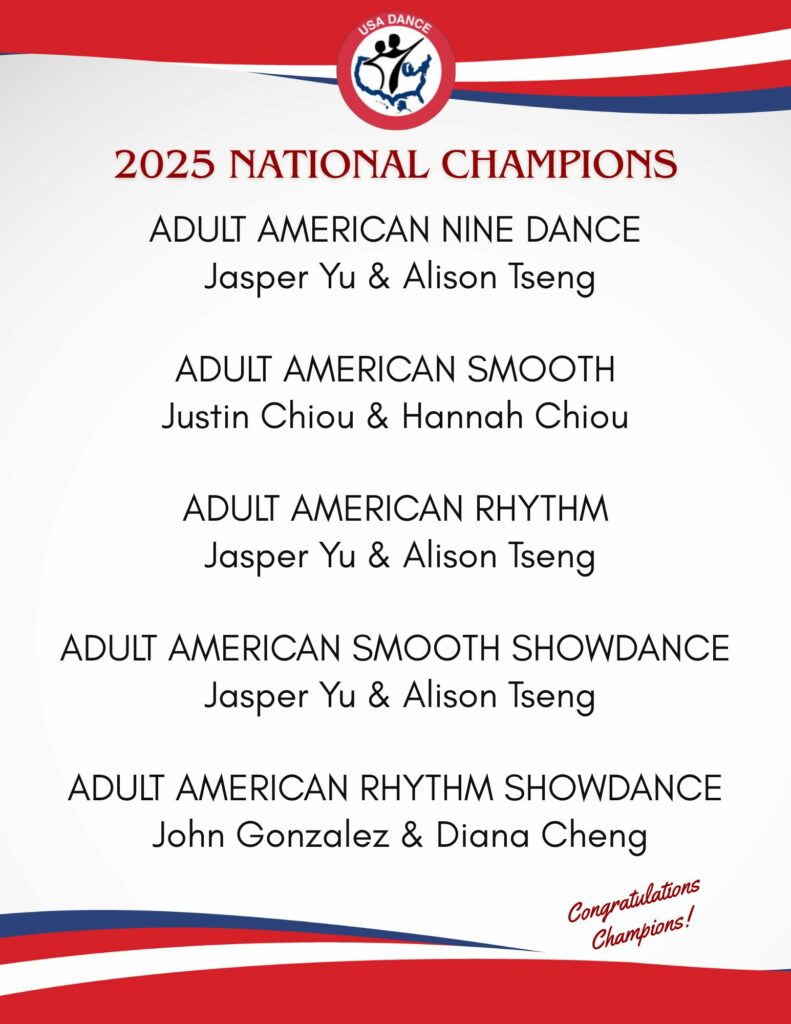
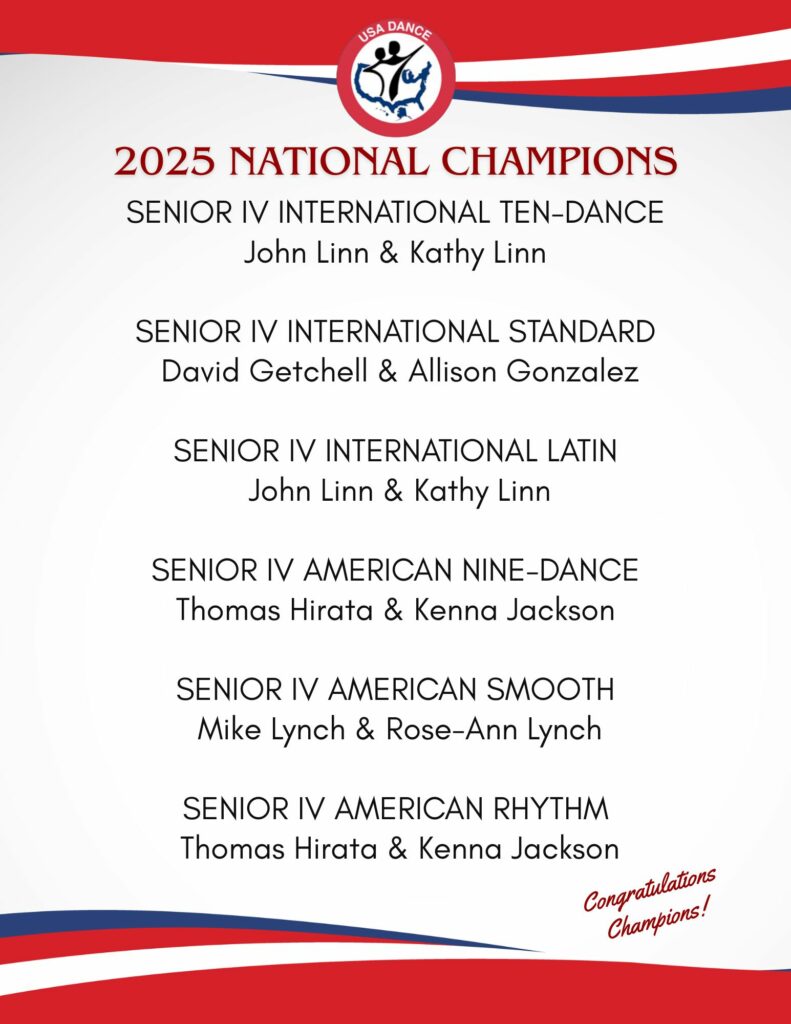
Editor’s Note: Read about one of our National Champions’ experiences with a knee replacement by Dr. Stone at the Stone Clinic. Senior III Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. Mike also provides a checklist to help you if you travel for surgery.1
Dr. Stone is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!