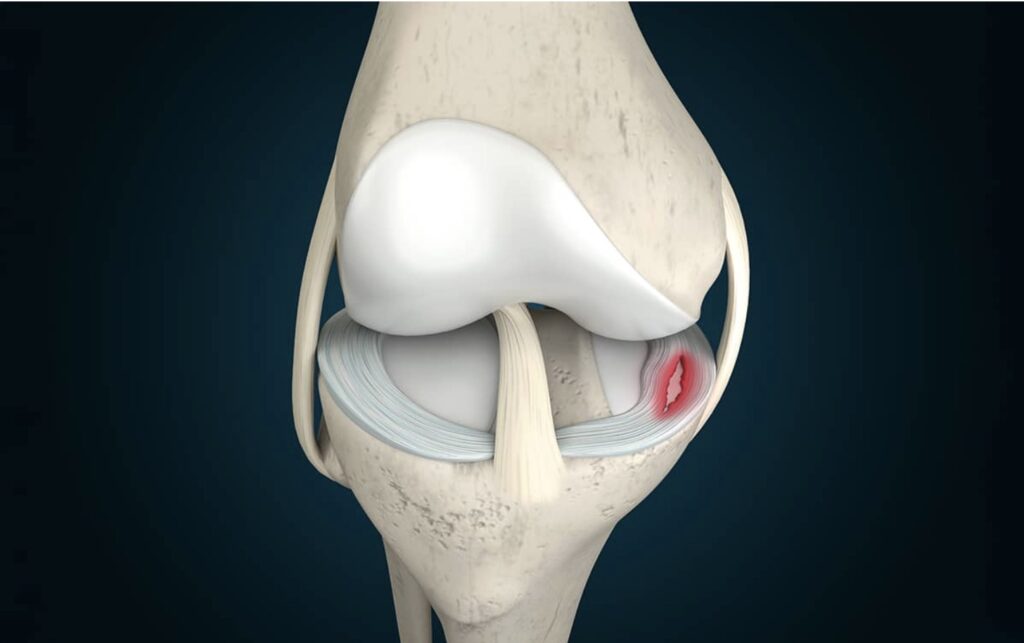
The meniscus is the key shock absorber in the knee joint. Torn 800,000 times a year in the US alone, it is a major cause of disability.
The meniscus is a fibrous tissue sitting between the femur and the tibia (shinbone). Since we take 2-3 million steps per year in normal walking, the meniscus takes a huge amount of force and distributes it smoothly across the tibial surface. Once torn, those forces are concentrated on a smaller area of the tibia, leading to overload and eventually arthritis.
The torn, fibrous meniscus tissue exposes its collagen fibers to the knee joint’s synovial fluid (the joint space lubricator). Cells—some of them stem cells—rush from within the injured meniscus, from the synovial lining, and from the fluid itself to initiate the repair process. It usually fails, most likely due to the forces and rotations of the knee that keep the edges of the tear apart.
If treated early, the freshly torn tissue can usually be repaired with sutures and the repairs augmented by cells from the bone marrow or blood clot made from the patient’s peripheral blood. Even old tears can be freshened up with a shaver and repaired. It used to be thought that only the outer portion of the meniscus—where the best blood supply exists—could be saved. But techniques for repairing most meniscus tears are now available. The desires of the patient, the skill of the surgeon, and the realities of insurance, work, life, and sports often determine which treatment is applied.
The sciences of meniscus repair, biology, biomechanics, and regenerative medicine have advanced dramatically. Scaffolds of collagen can be used to regrow missing sections, while donor tissues are available to fully replace the meniscus when it is lost due to injury, surgery, or arthritis.
Yet the practice of deploying each of these more advanced techniques is remarkably low. Eighty percent of all meniscus tears are resected and not repaired, regenerated, or replaced, even in the United States. The loss of tissue dooms the knee.
We don’t know how to change this. The science is clear, the techniques are taught at every orthopaedic meeting, and the tools are available. But the short-term benefits of resection—which include low cost, an early return to work and sports, and ease of technique—trump all the benefits that we know patients would receive from the newer techniques.
Having spent a lifetime on the science of tissue regeneration, I do know that the need for restoration of normal anatomy will not decline. As the benefits offered by new strategies continue to demonstrate success, the adoption of these techniques should become irresistible.
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.
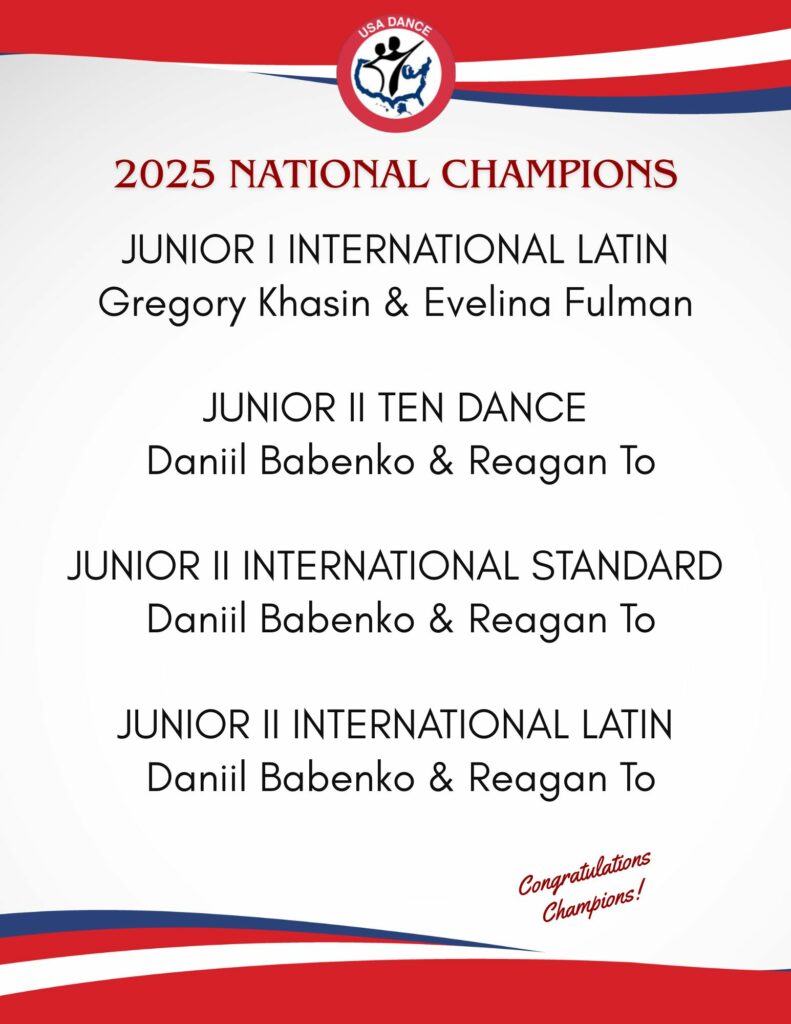
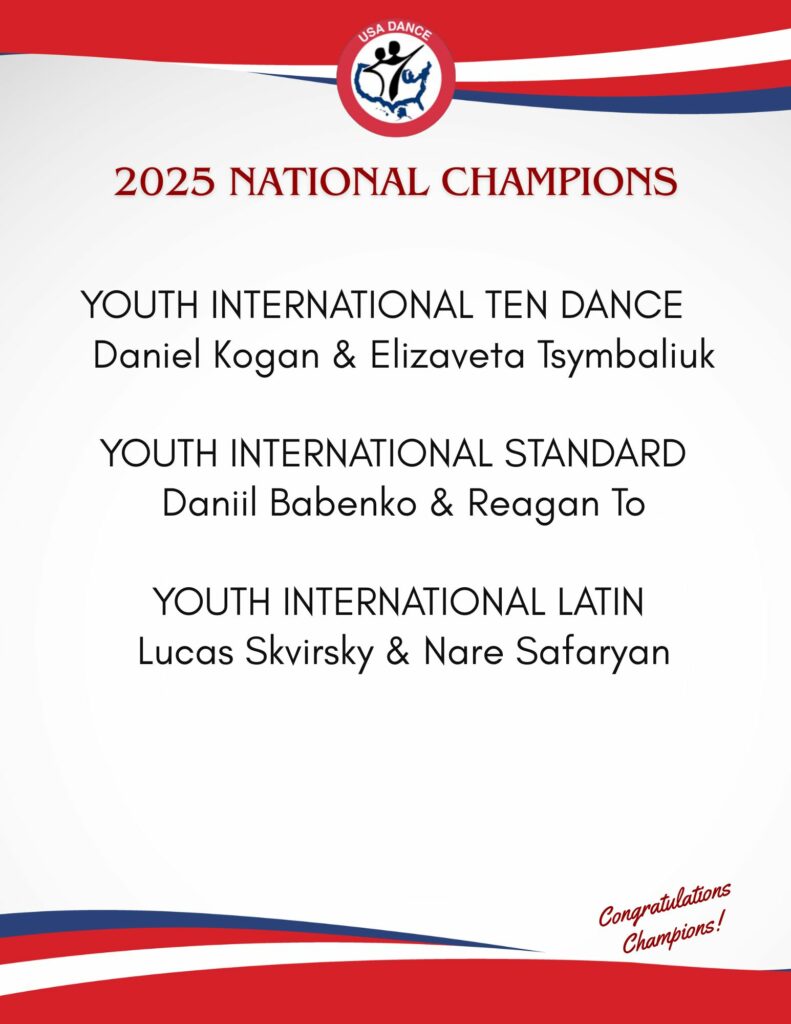
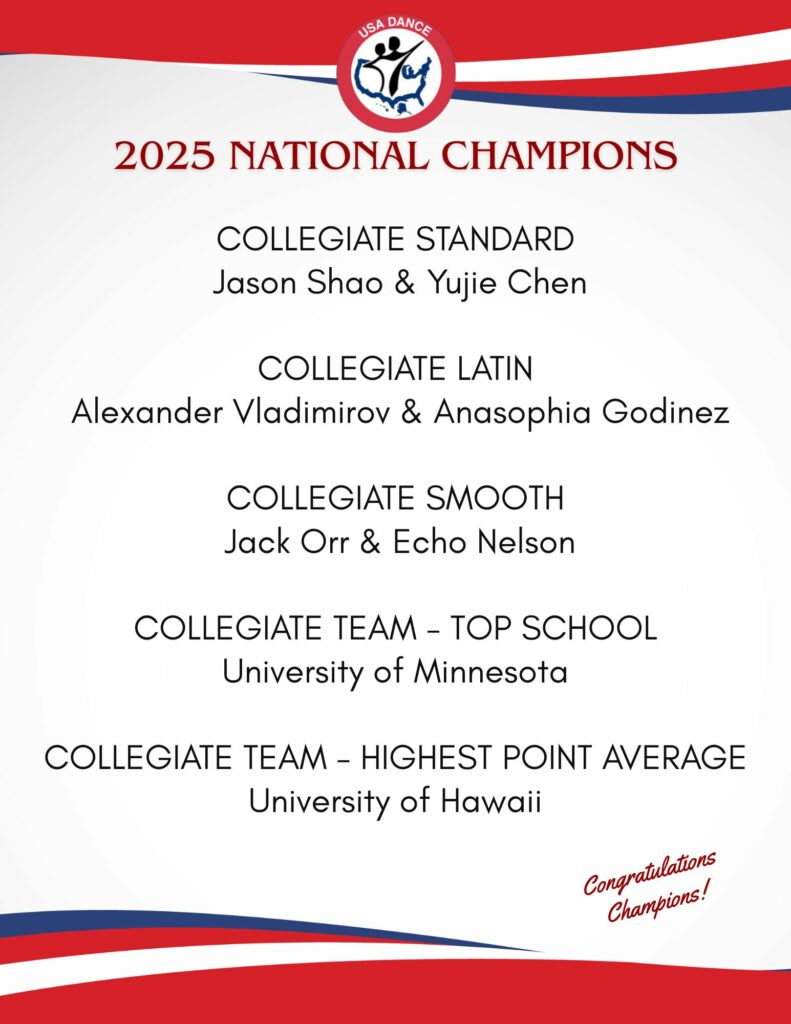
Editor’s Note: Read about one of our National Champions’ experiences with a knee replacement by Dr. Stone at the Stone Clinic. Senior III Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. Mike also provides a checklist to help you if you travel for surgery.1
Dr. Stone is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!