The choice to have an orthopaedic surgical procedure has many facets. Here are a few decision trees that make sense for the knee joint.
Deciding when to have something repaired versus just rehabilitating it non-operatively is sometimes challenging and sometimes straightforward.
Here are six points to consider: It is important to have surgery when you are sure of the diagnosis, the tissues injured can be treated effectively, the non-operative options are not good enough, your confidence in your ability to rehabilitate is high, your belief in the biases and skills of your surgeonare super high, and you are optimistic about your outcome. Otherwise, delay.
A few stories:
“Doc, I twisted my knee, heard a pop, and my knee swelled.” This is 90% of the time a surgically repairable problem such as a torn meniscus cartilage, a damaged ligament, or damaged articular cartilage (the bearing surface of the joint). If repaired early, each of these critical tissues can be saved and the knee joint returned to full activity. Untreated, arthritis often sets in.
“Doc, I have bone-on-bone arthritis and was told to give up sports, stay home and rest my knee, or just bike and swim—both of which I hate.” Here the patient has a choice. Many first try a cocktail injection: a mixture of the lubricant hyaluronic acid and PRP (Platelet-Rich Plasma), growth factors present in their own blood. Even with bone-on-bone arthritis, these injections—when combined with a great rehab program—often allow them to enjoy the ski season. The strategy is so effective that I commonly hear “Doc, I won’t let you fix my knee until those lube jobs stop working!”
When the bone-on-bone knee arthritis is causing pain and loss of motion and not responding to lube jobs and rehab, it is time to repair it. Still, a huge number of people who were told they need a total knee replacement might be able to have a biologic solution. This involves replacing the missing tissues and repairing the articular cartilage. A partial knee replacement requires less surgery, and results in a more normal-feeling knee, better range of motion, and an earlier return to full sports.
“Doc, my kneecap is loose. It used to dislocate, and now just hurts.” Anterior knee pain (i.e., pain in the front of the knee) can be the most difficult to diagnose, deduce the cause, and treat. And living with anterior knee pain is difficult, as every time you go up and down stairs or walk and hike the hills, your knee talks to you.
Muscle strengthening, knee braces, taping, and gait training are employed by almost every therapist. These strategies are sometimes effective, yet patients rarely comply enough to make a big difference. If the kneecap is unstable, a ligament reconstruction procedure using a donor graft can stabilize the kneecap. Our ballet dancers and hyper-mobile athletes are the most common recipients of this treatment.
If the kneecap is arthritic and has bone-on-bone grinding, either a cartilage repair procedure or a partial knee replacement for just the patella femoral joint is quite effective in restoring pain-free function. If the arthritis is not too bad, and the cartilage is just frayed, simple smoothing of the tissue, combined with lubrication and growth factor cocktails, can often solve it.
“Doc, my knee buckles and gives way when twisting.” Instability in life and in knee joints leads to bigger problems. Fortunately, all of the knee joint ligaments, if freshly torn, can be repaired or reconstructed with your own or donor ligament. The techniques are now often combined with using factors to recruit your own stem-cell-derived repair cells. This can speed up a return to full sports.
“Doc, my knee locks and has hurt on the joint line since I had part of my meniscus removed. Isn’t there just a shock absorber you can put in my knee?” Even small sections of loss can lead to significant arthritis. A torn meniscus should be repaired if at all possible, and replaced if necessary. It can be replaced later in life as well. Our recent data shows that, in many cases, doing this can delay and often eliminate the need for an artificial knee replacement.
So: Get an early, accurate diagnosis, then treat with non-operative methods when critical tissues are not at risk. Surgically repair, reconstruct, or replace when tissues are dysfunctional. Millions of years of evolution gave you those tissues for a reason. A few decades of surgical skill improvements can now give them back to you.
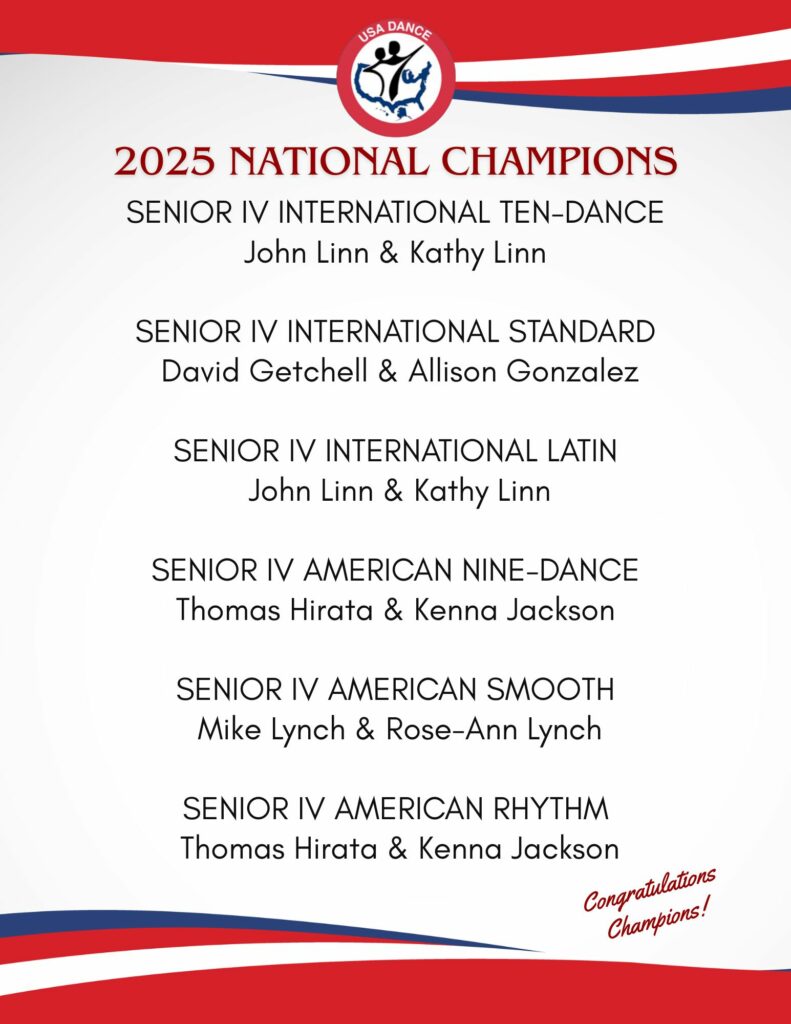
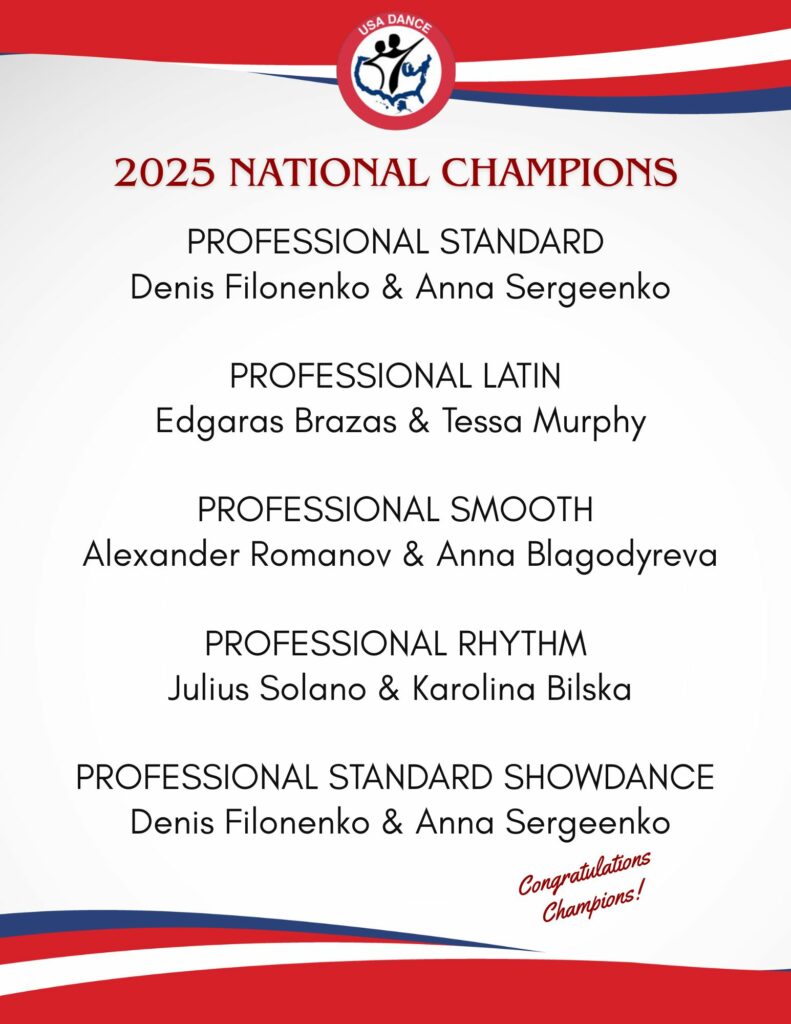
Editor’s Note: Read about one of our National Champions’ recent experiences with a knee replacement. Senior III Smooth and Standard Dancer Mike Lynch talks about his injury, research, procedure, therapy, and progress. He also provides a checklist to help you if you travel for surgery.
 Kevin R. Stone, MD
Kevin R. Stone, MD
Dr. Kevin R. Stone is a pioneer of advanced orthopaedic surgical and rehabilitation techniques to repair, regenerate, and replace damaged cartilage and ligaments.
He is an orthopaedic surgeon at The Stone Clinic and also the chairman of the Stone Research Foundation. He lectures around the world as an expert in cartilage and meniscal growth, replacement, and repair and holds over 40 U.S. patents on novel inventions to improve healthcare.
Dr. Stone uses anabolic therapy and other biologic techniques to work to preserve the natural biology of a joint, helping people avoid or delay an artificial joint replacement.
At The Robotic Joint Center, Dr. Stone uses advanced robotic-assisted surgery techniques to ensure that partial and total knee replacements result in precise alignment and a more natural feeling knee
Dr. Stone was trained at Harvard University in internal medicine and orthopaedic surgery and at Stanford University in general surgery. His fellowship was in research at the Hospital for Special Surgery and in knee surgery in Lake Tahoe. Dr. Stone is consistently listed as one of the country’s top 25 Ambulatory Surgery Center (ASC) leaders and ranks amongst the country’s top 75 knee surgeons.1
He is a physician for Smuin Ballet and has served as a physician for the U.S. Ski Team, the U.S. Pro Ski Tour, the Honda Ski Tour, the Jeep 48 Straight Tour, the Old Blues Rugby Club, Lawrence Pech Dance Company, Marin Ballet, the modern pentathlon at the U.S. Olympic Festival, the United States Olympic Training Center, and for the World Pro Ski Tour. He’s been featured on Good Morning America, the Ologies podcast, and Star Talk podcast hosted by Neal deGrasse Tyson. He is the best-selling author of the book Play Forever. He also served as a columnist for the San Francisco Examiner and writes a weekly blog at www.stoneclinic.com/blog.
Dr. Stone enjoys skiing, windsurfing, and biking.
This article was reprinted with the express permission of Dr. Kevin Stone, MD and The Stone Clinic. To see or sign up for The Stone Clinic’s Blog, Click Here!